Risk of secondary cancer after CAR-T cell therapy is low, according to major Stanford Medicine study
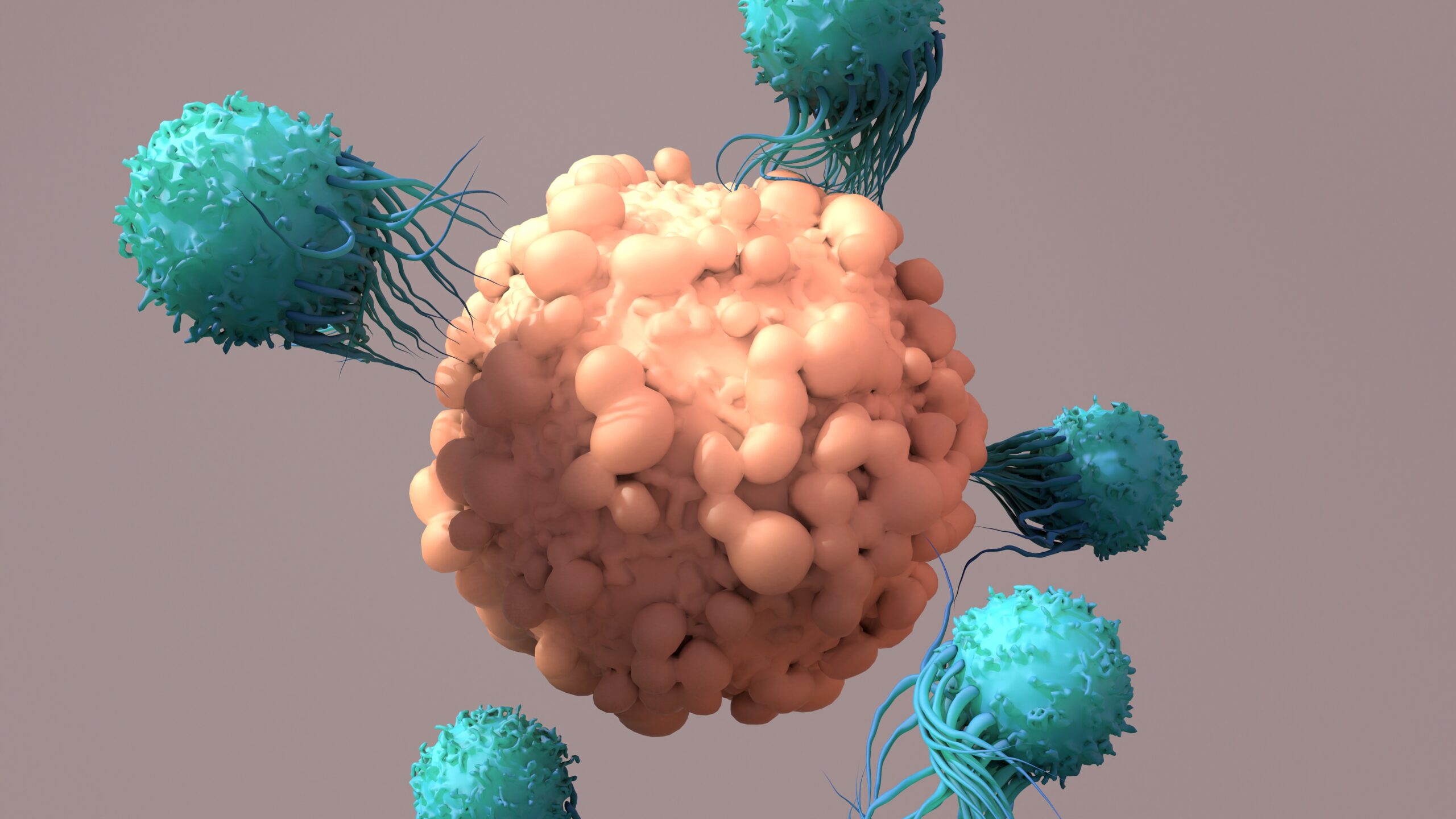
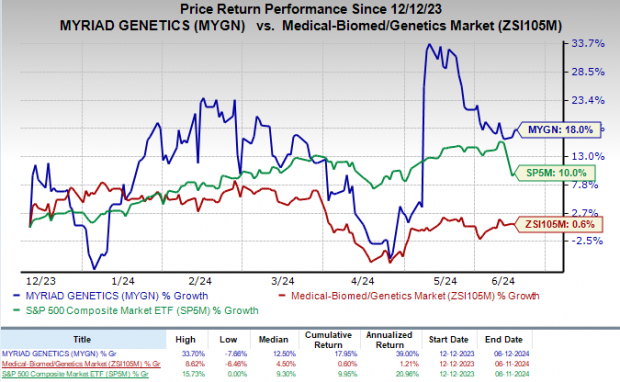
Researchers analyzed outcomes for 724 people treated with CAR-T cell therapy at Stanford Health Care between 2016 and 2024. Among these people, the incidence of secondary blood cancers approached 6.5% during an average of three years of follow-up, which is roughly similar to patients who underwent stem cell transplants instead of CAR-T cell therapy to treat their cancer. Only one person rapidly developed and died from a T-cell cancer called T-cell lymphoma shortly after CAR-T cell therapy.
The researchers used molecular, cellular, and genetic analyzes — including several new genetic profiling techniques developed in Alizadeh’s lab — to compare all of the 724 patients’ tumors, their CAR-T cells, and their healthy cells at several points. time before and after CAR-T cell treatment. .
“This was a herculean effort by the study’s first authors, working feverishly as a team from just before Thanksgiving until Christmas,” Alizadeh said.
The analysis found no evidence that the T cells responsible for the patient’s second cancer were T cells engineered for CAR-T cell therapy – they were molecularly and genetically distinct. However, both sets of T cells were infected with a virus known to play a role in the development of cancer. Additionally, the patient had a history of autoimmune disease in the years before the first cancer diagnosis.
The study’s findings suggest that secondary cancers that arise after CAR-T cell therapy may be due to underlying immunosuppression or side effects of the treatment, rather than the erroneous insertion of the chimeric antigen receptor gene during genetic engineering of the T cells. .
“These results may help researchers focus on the immune suppression that can precede and often follows CAR-T cell therapy,” Miklos said. “Understanding how it contributes to cancer risk is particularly important as the CAR-T cell field shifts from treating high-risk, refractory blood cancers to lower-risk but clinically relevant disorders, including autoimmune.”
“This study can serve as a blueprint for how to capture and characterize the results of CAR-T therapies so that we can develop a very clear understanding of their risks and benefits,” Alizadeh said. “These are life-saving therapies that come with a very low risk of secondary cancer. The challenge is how to predict which patients are at higher risk and why.”
The study was funded by the National Institutes of Health (grants R01CA233975, NCI P01 CA049605), the Leukemia and Lymphoma Society, the Lymph&Co Foundation, the Virginia and DK Ludwig Fund for Cancer Research, Kite-Gilead, and Adaptive Biotechnologies.
See also:
Stanford Cancer Institute
#Risk #secondary #cancer #CART #cell #therapy #major #Stanford #Medicine #study
Image Source : med.stanford.edu